Virtual OSCEs, a First at LAU and in Lebanon
Inter-departmental efforts realize the first virtual OSCE exams at LAU’s School of Medicine.
As COVID-19 struck toward the end of the academic year, the pressure was on for faculty to ensure that students complete their semester and that seniors graduate. For certain courses, the shift to online delivery was facilitated by existing digital platforms, while for others it called for innovation, especially when it came to standardized final exams.
At the Gilbert and Rose-Marie Chagoury School of Medicine (SOM) where a rigorous assessment of Med IV students for clinical competency is a must to ensure patient safety, the pandemic presented significant challenges.
“Not only was it critical to ensure final-year students are not delayed in their graduation and their entry to the clinical workforce in times of a healthcare crisis,” said Professor of Nephrology and Associate Dean for Medical Education Sola Aoun Bahous, “but also that they are assessed to determine their competency and maintain performance standards.”
To meet these requirements, added Dr. Bahous, and as a first in Lebanon, the SOM had to conduct the Objective Structured Clinical Examination (OSCE) virtually.
OSCE is designed to test clinical skill performance and competence in a range of skills such as communication skills, physical examination techniques, professionalism, and abilities to effectively interact with patients and other healthcare workers. “As one of the most widely used performance-based assessments in undergraduate, postgraduate and licensing assessments, when performed properly OSCE is valid, reliable, and fair and therefore suitable for use in high-stakes assessments,” explained Dr. Bahous.
During a typical OSCE, students rotate through a series of timed stations where a specific clinical scenario assesses one or more areas of clinical competence, such as history taking, communication, physical examination skills, etc. The OSCE process involves the use of simulated patients (SPs), who are trained actors, in simulated clinical scenarios. Faculty evaluators observe each student’s performance in the standard scenarios to assess specific knowledge, skill performance, and clinical reasoning using standardized rubrics.
“The use of standardized cases and rubrics allows for an objective evaluation of student competencies, which is not always possible in real-life clinical scenarios,” explained Dr. Nadia El Asmar, OSCE director and associate director of the Clinical Simulation Center (CSC).
Migrating to virtual OSCEs was far from straightforward for the team composed of Dr. Bahous; Dr. Vanda Abi Raad, clinical professor of anesthesiology and director of the CSC; Dr. El Asmar; Dr. Lina Abyad, associate professor at the School of Arts and Sciences, who was responsible for training the SPs; the IT Department; CSC coordinators; and SOM staff and faculty.
Following brainstorming sessions, attending webinars and exhausting all possibilities, the OSCE team soon realized that “the literature was scarce, as other international medical schools were facing the same challenge, and we would have to come up with our own format while being imaginative and flexible,” said Dr. Abi Raad.
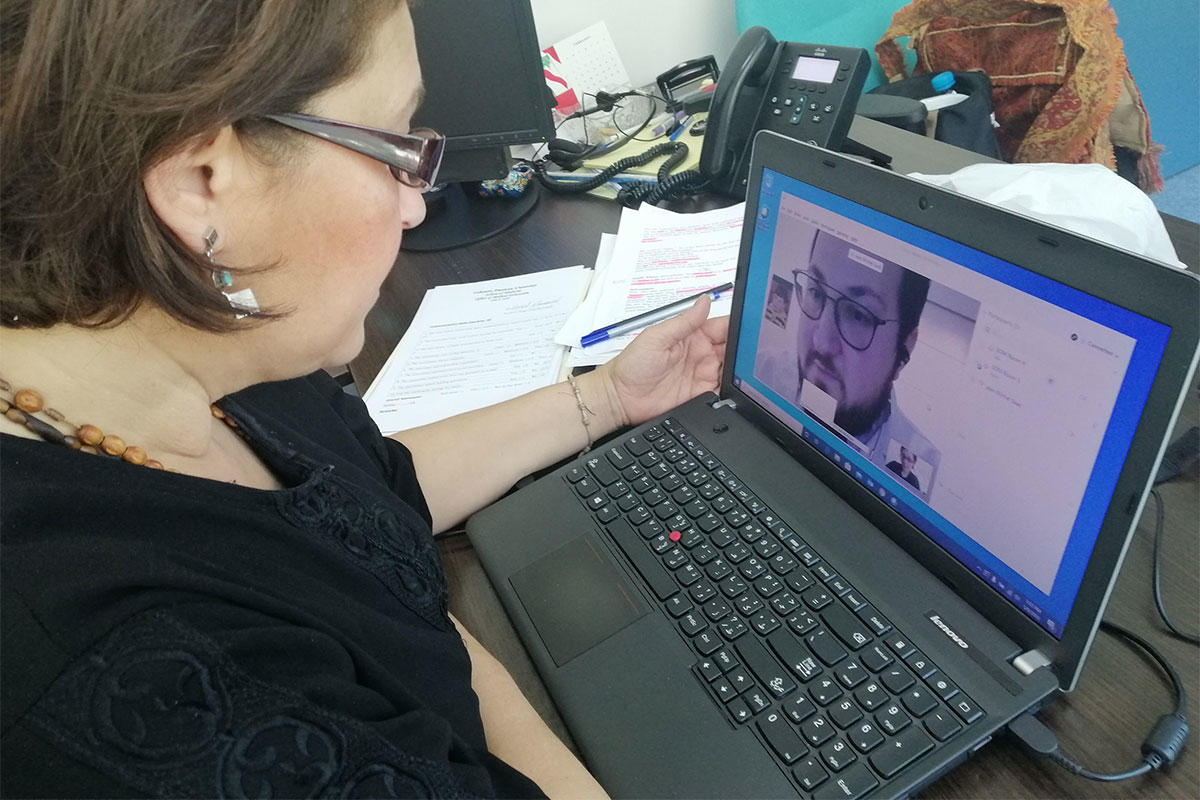
The challenges were many: “To devise an OSCE structure where SPs, students and faculty are not physically co-located; simulate virtual visits and train SPs and faculty through telehealth; find a suitable technical platform; and schedule appointments with students quarantined in Lebanon and others in different time zones,” explained Dr. El Asmar.
To overcome these hurdles, students’ encounters with SPs were done through a videoconferencing tool, while faculty evaluators kept their microphones muted and videos switched off. With the help of the IT department, the team was able to use various platforms concomitantly: Webex, Blackboard and Learning Space, an advanced audiovisual system acquired some time ago through a generous ASHA grant. And, finally, to cater to all students, the OSCE was carried out in two consecutive sessions, morning and afternoon.
The feedback received from the students, which they submitted in an anonymous evaluation form after sitting for the examination, was extremely positive. Commending the expedient delivery of virtual OSCEs, the students remarked that it was a valuable exposure to telemedicine, which is becoming common practice across all specialties.
Given the time and effort invested in developing virtual OSCEs, and their success, could they be used in the future? “The COVID-19 pandemic brought telemedicine into a new light and the need for remote technologies skyrocketed,” said Dr. Abi Raad. “It seems that the use of telemedicine will continue to flourish to a certain degree after COVID-19, so having a hybrid OSCE system that includes onsite and virtual stations would be a good approach in the future.”
Maintaining the highest level of education is paramount, especially when it comes to patient safety, said SOM Dean Michel E. Mawad. “Even in times of crisis, it is vital that we ensure that medical standards are met. There is no question of a compromise when patient safety is at stake. And I’m happy to say that, thanks to our resourceful and diligent faculty, we are able to graduate students who are up to the task.”