Food and the Fight Against Cancer
Dr. Jana Jabbour underscores the relationship between diet and cancer risk and advocates for lifestyle and policy modifications to combat obesity for overall wellbeing.
On November 15, the School of Arts and Sciences (SoAS) held a lecture by Assistant Professor of Nutrition Jana Jabbour titled Nutrition and Cancer Prevention–The Good, the Bad and the Ugly as part of the SoAS Lecture Series. The talk addressed how our daily dietary choices can impact the likelihood of cancer progression and provided practical dietary recommendations for enhancing overall health.
This article highlights key takeaways from the discussion, based on evidence from scholarly articles and Dr. Jabbour’s research projects.
What are some dietary components that decrease cancer incidence?
We often hear that whole grains and fiber are good for you. In fact, both have also been linked to a reduced risk of colorectal cancer, and fiber has been proven to help control weight gain and obesity.
Whole grains contain three components: The bran, endosperm and germ. In contrast, refined grains – like white bread, regular pasta or sugar – only retain the endosperm after processing, resulting in a loss of essential nutrients such as fibers, magnesium, selenium, folate, vitamin E and phytochemicals – bio-active compounds that provide health benefits without the extra calories.
Incorporating whole grains into a diet is proven to offer a nutritional powerhouse rich in nutrients and good protection against the risk of cancer.
Coffee also boasts antioxidants and metabolites and acts as a defender against inflammation and cell damage. It is recommended, however, not to exceed 400 milligrams of caffeine per day, about 4-5 cups of espresso or tea, to identify other sources of caffeine, such as energy and soft drinks, and to avoid having it with sweeteners or tobacco.
What are the eating habits, or bad dietary components, that can increase the risk of cancer?
Top of the list is overconsumption of ultra-processed foods, which accounts for 50 to 60 percent of calories in the UK, Canada and the US for instance. Industrially processed food items, such as refined grains, soft drinks, processed meat and margarine, contribute to a 12 percent increase in the overall risk of cancer for every 10 percent rise in consumption.
High sodium intake, which is common in foods like bread, pumpkin seeds or chips, can damage the stomach lining. One of the reasons behind the overconsumption of sodium is the misleading product labels. Consumers would understand that a “reduced sodium” label means the product has 25 percent less sodium than the regular one, but it does not mean it’s low in salt. The World Health Organization recommends limiting sodium intake to 2.3 grams, or around 1 teaspoon, a day.
Overconsumption of alcohol is another culprit. While moderate alcohol intake raises the risk of cancer by 80 percent, heavy or binge drinking increases the risk by 500 percent, particularly for mouth, throat, esophageal, breast, colorectal and liver cancers. Despite associations with decreased risk for kidney cancer and non-Hodgkin lymphoma, the overall risks of alcohol consumption outweigh the benefits due to its diverse impact on the body.
As for meat, boosting daily red meat intake by 100-150 grams raises colorectal cancer risk by 12-17 percent. Processed meats, with added nitrites and nitrates during curing, spike pancreatic cancer risk by 49 percent while their fat content raises secondary bile acids, upping the cancer risk.
People have heard that obesity is linked to cancer, but how does the issue factor into the equation?
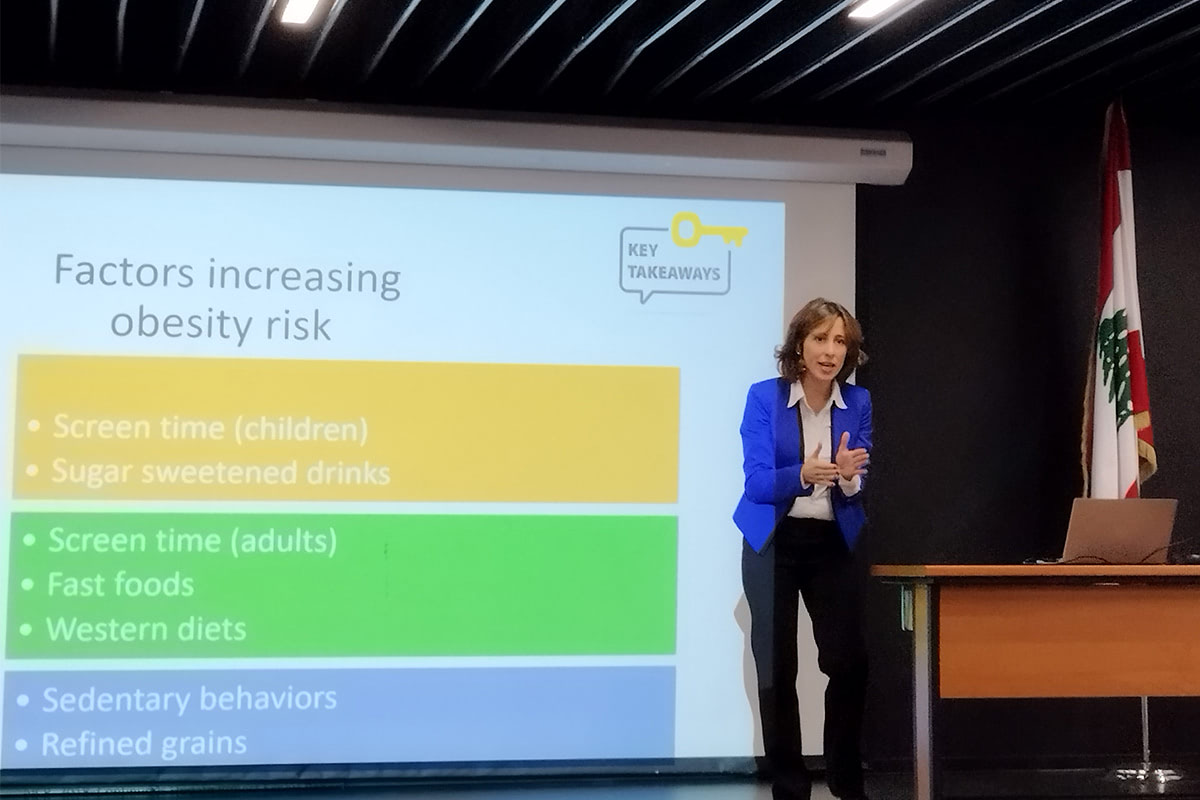
Obesity is a significant, modifiable risk factor for more than a dozen types of cancer after smoking. Adipose tissue or body fat acts as an active organ, producing hormones and inflammatory substances that can influence cell growth, immune function and insulin sensitivity. An elevated adipose tissue percentage creates an environment conducive to cancer development.
In Lebanon, around 55 percent of our adult population is either overweight or obese. It gets worse among children as estimates show that two out of 10 kids under five are already overweight.
Underlining specific types of cancer associated with obesity and unhealthy eating habits, including breast, colorectal, pancreatic and esophageal cancers, entails advocacy in lifestyle modifications to combat obesity, thereby reducing cancer development.
What lifestyle modifications do you advocate for in combating and reducing cancer risk?
Adopting a balanced, nutrient-dense diet, engaging in regular physical activity and maintaining a healthy weight.
Consider behavioral therapy when necessary, focusing on mindful eating. Implement in parallel a Mediterranean diet rich in fibers – nuts, fish and whole fruits – while minimizing fried and junk food.
Don’t let the sedentary habits linger, even after a power-packed hour of exercise. Stay active throughout the day. This applies to both children and adults.
Ultimately, overall wellbeing involves more than the individual and goes beyond cancer prevention. We need policies, communities, institutions and organizations to promote healthy choices by implementing effective frameworks that support and incentivize individual and collective behavior.
A healthy lifestyle positively impacts various facets of one’s health, from cardiovascular to mental health. So, the key is a balanced and informed approach to nutrition and lifestyle choices.