How to Sleep Better Despite Stressful Circumstances
LAU health professionals tackle sleep disruptions, question melatonin’s effectiveness for sleep disorders and provide strategies for restful sleep amid heightened stress.
Most healthy adults need about seven hours of quality sleep each night. However, with increased stress levels, restful sleep becomes harder to attain for individuals of all ages, which negatively impacts their physical and mental well-being.
In response to this growing issue—made more acute by recent events—the LAU Gilbert and Rose-Marie Chagoury School of Medicine’s Office for Continuing Medical Education (CME) and the School of Arts and Sciences (SoAS) hosted the fifth installment of their joint psychotherapy webinar series, titled Restless Minds: Unpacking Sleep Disorders in a Stressed-Out World, on November 6.
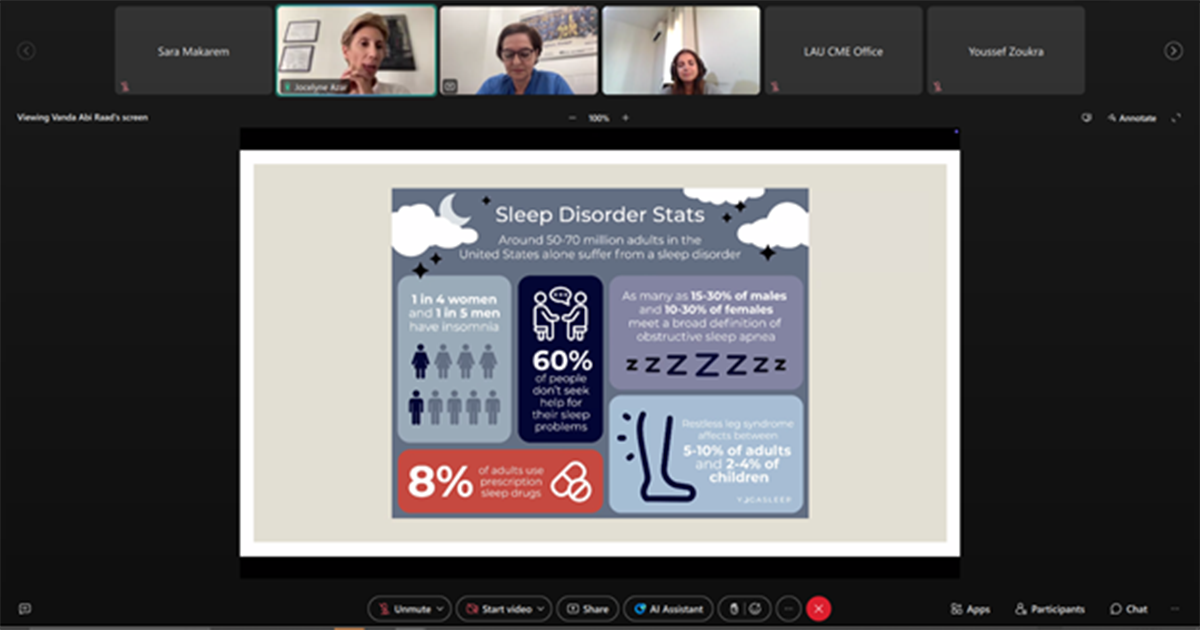
“There is a bidirectional relationship between sleep and mental health,” explained Clinical Assistant Professor of Psychiatry Jocelyne Azar. Stress can trigger sleep disturbances such as insomnia, hypersomnia, sleep apnea, narcolepsy, restless leg syndrome and parasomnias. In turn, these disturbances can amplify stress. Dr. Azar noted that sleep disorders often warrant a closer look, as they may signal underlying stress-induced psychiatric conditions, including depression, anxiety, PTSD and bipolar disorder.
Additionally, she cautioned about the physical, psychological and social consequences of untreated sleep disturbances, both in the short and long term, which include an increased risk of cardiovascular disease, obesity, immune dysfunction, cognitive impairment, memory loss, strained relationships and reduced productivity.
To help create better sleep hygiene, Assistant Professor of Psychology at SoAS Marie Anne El-Khoury outlined various factors that typically impact sleep quality and duration, including environmental elements like temperature, lighting, bedding and noise. Also affected are behavioral habits such as phone use, eating, or exercising close to bedtime; physiological influences like hormonal levels and respiration; and cognitive factors, such as stress, alertness and anxiety.
Reducing sleep-related rumination was one of the 12 sleep hygiene tips Dr. El Khoury shared with attendees. “Journaling helps process the events of the day, significantly easing nighttime rumination that can keep us awake,” she said. Other tips included establishing a bedtime routine and reducing mental stimulation before sleep.
“Don’t overwhelm yourselves by trying to follow all sleep hygiene practices at once,” she advised. “Try different approaches, see what works best for you, and go with that.”
Among the questions addressed to the speakers was one on the efficacy and safety of melatonin use in managing sleep disorders, to which Dr. Azar responded that “while melatonin is a popular supplement, it primarily helps regulate the circadian rhythm rather than inducing sleep like traditional sleeping pills.” She emphasized that while it can be effective for adjusting sleep after jet lag or for people with delayed sleep issues, it’s only recommended for short-term use—about one to two months—”since prolonged treatment may inhibit the body’s ability to self-regulate sleep.”
Similarly, in response to a question about using magnesium to relieve anxiety, Dr. Azar noted that it can be beneficial in alleviating symptoms of mild anxiety. However, when insomnia occurs alongside depression and heightened anxiety, magnesium serves only as a supplement to psychological or psychiatric therapy.
To wrap up, Dr. El Khoury shared video links to mindful practices that can be incorporated before bedtime. She acknowledged that these psychotherapy webinars are not solutions to the multiple crises facing the country but are intended to “help reduce their impact on our health and improve sleep quality amidst these challenges—more a matter of damage control than complete solutions.”
To view the recording of this session, please click here.