The Crucial Role of Anesthesiologists in Mass Casualty Response
LAU alumni share their frontline experiences as anesthesiologists in conflict zones, highlighting best practices and the vital role their profession plays during emergency responses.
As part of the 2024 Special Grand Round Series showcasing the exceptional achievements of LAU alumni, the Office of Continuing Medical Education at the LAU Gilbert and Rose-Marie Chagoury School of Medicine hosted its 16th session on October 17, featuring young LAU professionals who have made significant strides in the field of anesthesiology.
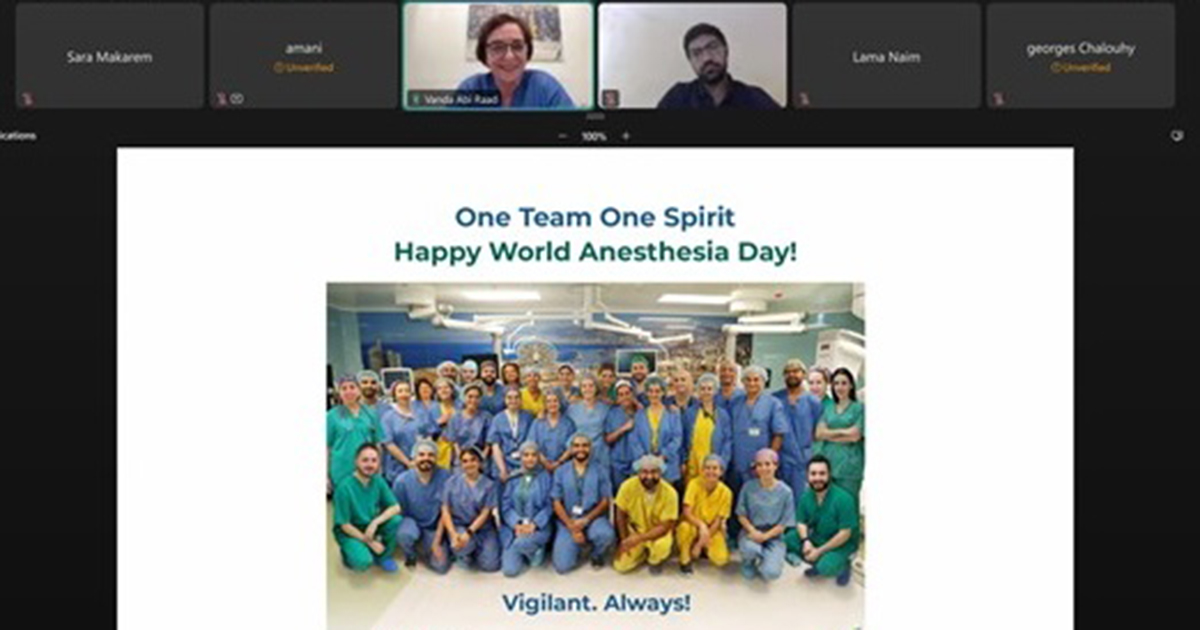
The event coincided with World Anesthesia Day, celebrated annually on October 16 by the World Federation of Societies of Anesthesiologists (WFSA).
Titled Anesthesiologists at the Heart of Mass Casualty Response: A Rich History, A Busy Future, the online event was led by Dr. Amani Jaber (MD ’14), head of the anesthesiology department at Al Rassoul Al Aazam Hospital and Dr. Alaa El Chal (MD ’17), fellow in cardiovascular and thoracic anesthesia in the department of anesthesia and intensive care at Limoges University Hospital, who shared their advanced knowledge, experiences and challenges in Mass Casualty Incidents (MCI), highlighting the critical role anesthesiologists play.
In addition to their expertise in pain management, anesthesiologists perform vital clinical responsibilities such as airway control, hemodynamic monitoring, fluid resuscitation, critical care and patient rapid assessment. These skills make them key collaborators with ER, ICU, OR and surgical doctors and nurses in times of disaster response.
“Despite all the challenges, our Lebanese anesthesiologists work and serve as a testament to the resilience and compassion that define our profession,” commented Dr. Vanda Abi Raad, associate dean for faculty affairs and development at the school of medicine, moderator of the online meeting and clinical professor and chair of the Department of Anesthesiology at the LAU medical centers.
Speaking to attendees from the school of medicine and the broader medical community, Dr. Jaber outlined the many types of injuries anesthesiologists handle during emergency responses, including blunt trauma from building collapses, penetrating trauma from gunshot wounds and shrapnel, burns, crush injuries, blast injuries and psychological trauma such as Acute Stress Disorder and PTSD.
Drawing from her experience treating casualties of the recent pager bombings in Lebanon, Dr. Jaber emphasized the pivotal role anesthesiologists play in triaging and stabilizing patients’ influx into the ER. “We act as a vital link between the emergency department and the operating room, particularly in assessing patients and determining whether they need to be transferred to other departments,” she explained.
“The only way we can effectively manage this wide range of traumas is by adhering to an established protocol tested in emergency drills and reinforced through simulation-based training,” she added.
In turn, Dr. El Chal discussed the challenges anesthesiologists face during chemical attacks, highlighting the clinical symptoms they monitor, the incident response protocols and treatment options for major chemical agents like hydrogen cyanide and mustard gas. He emphasized the critical need for institutional and professional preparedness, as well as blood bank readiness, along with interdisciplinary collaboration during such attacks.
“As intraoperative intensivists, anesthesiologists can offer a great deal during MCIs,” he explained. “In addition to assisting with patient triage, they perform multiple and simultaneous procedures to manage patients and address life-threatening conditions.”
Building on this, Dr. Chal emphasized the importance of institutional debriefing after disaster responses to assess performance, recommend improvements and refine protocols, ensuring continuous enhancement in handling such critical situations.
Toward the end of the online session, during the discussion period, Clinical Assistant Professor of Psychiatry Wael Salame—who was among the attendees—weighed in suggesting that physicians, nurses and staff should also be given the opportunity for psychological debriefing. This would allow them to reflect on challenging cases and difficulties, helping them process the trauma encountered during such events.